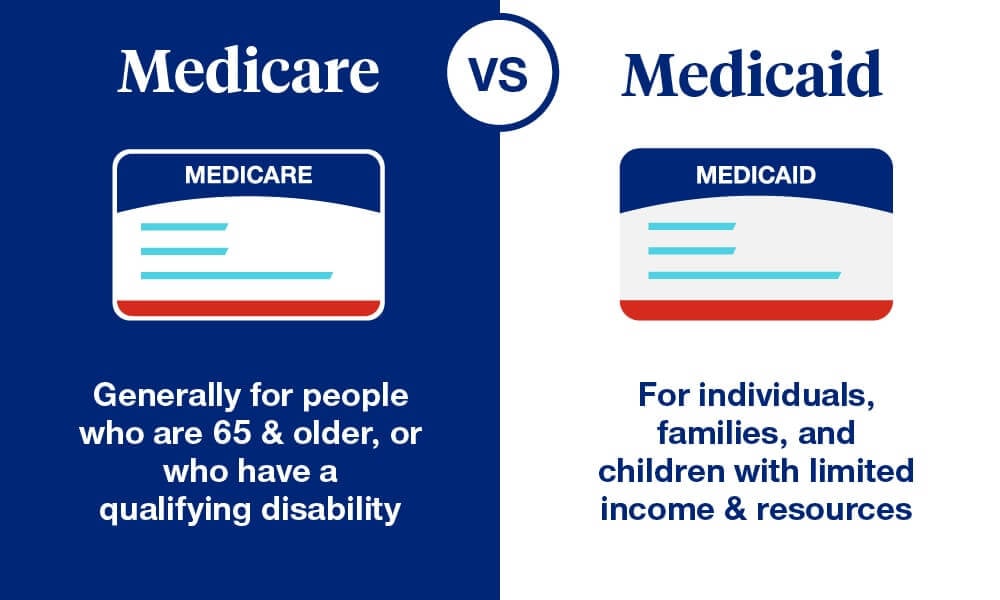
Medicare and Medicaid are two essential health programs in the United States that are paid for by taxpayers. They were both founded in 1965. They serve different populations and serve different goals while having similar names and origins. Their eligibility requirements vary according on age, income level, and other considerations. In order to help people navigate Medicare and Medicaid efficiently, this article will explain the distinctions between the two systems, with a particular emphasis on the income restrictions, eligibility conditions, and coverage details of each.

Medicare: Federal Health Insurance for Seniors and Disabled Individuals
Medicare is a federal program providing health insurance primarily to people aged 65 and older, regardless of income, and to younger individuals with certain disabilities. The program consists of several parts:
- Part A (Hospital Insurance): Covers inpatient hospital stays, care in nursing facilities, hospice care, and some home health care.
- Part B (Medical Insurance): Covers certain doctors’ services, outpatient care, medical supplies, and preventive services.
- Part C (Medicare Advantage): Offers an alternative way to receive Medicare benefits through private insurance companies.
- Part D (Prescription Drug Coverage): Adds prescription drug coverage to Original Medicare, some Medicare Cost Plans, some Medicare Private-Fee-for-Service Plans, and Medicare Medical Savings Account Plans.
Medicaid: Joint Federal-State Program for Individuals and Families with Limited Income
Medicaid, as opposed to Medicare, is a combined federal-state program that assists some individuals with low incomes and resources with their medical expenses. Medicaid also provides services like personal care and nursing home care that are not often covered by Medicare. States can differ greatly in terms of eligibility requirements and specific coverage.
Key Differences Between Medicare and Medicaid
Funding and Administration
- Medicare: Funded primarily through federal funds and managed by the federal government.
- Medicaid: Funded by both state and federal governments but administered at the state level, allowing for variability in how Medicaid operates across different states.
Eligibility Criteria
- Medicare: Primarily age-based, with eligibility typically beginning at age 65. Younger individuals with disabilities or those with End-Stage Renal Disease (ESRD) or Amyotrophic Lateral Sclerosis (ALS) can also qualify.
- Medicaid: Primarily needs-based, focusing on individuals and families with low income. Eligibility varies by state, and some states have expanded their Medicaid programs under the Affordable Care Act to include a broader range of low-income adults.
Income Limits
- Medicare: There are no income limits to qualify for basic coverage; however, higher-income individuals may pay more for Medicare Part B and Part D premiums. For 2024, individuals with an income above $103,000 and couples above $206,000 will face higher premiums.
- Medicaid: Income limits are set at a percentage of the Federal Poverty Line (FPL), which can vary by state. For example, under the ACA expansion, many states cover all adults below 138% of the poverty level.
Transition from Medicaid to Medicare at Age 65
When Medicaid recipients turn 65, they generally become eligible for Medicare. The transition can affect their Medicaid coverage depending on their income:
- Higher-income individuals: Medicaid may only cover Medicare Part B premiums.
- Lower-income individuals: May continue to receive comprehensive benefits through Medicaid, which supplements Medicare coverage by paying for costs like copayments and deductibles.
The Impact of the Affordable Care Act
Expanding Medicaid eligibility was a primary goal of the Affordable Care Act (ACA), which was enacted to provide healthcare coverage nationwide. States were still free to decide whether to accept the Medicaid expansion, though, thanks to a ruling by the Supreme Court. As a result, there is a patchwork of eligibility requirements across the nation, with some states choosing not to expand Medicaid to cover additional adults with low incomes and others choosing to do so.
It is essential to comprehend the differences between Medicare and Medicaid in order to obtain the proper medical coverage. Both systems strive to offer health security, but they serve different populations and have different benefits and eligibility restrictions. Understanding these programs’ framework is necessary to navigate them efficiently, especially in relation to one’s healthcare demands and financial situation.
FAQs
Q1: Can someone be eligible for both Medicare and Medicaid?
A1: Yes, individuals who qualify due to age or disability for Medicare and meet the income requirements for Medicaid can be eligible for both, known as “dual eligibles.”
Q2: How does one apply for Medicare or Medicaid?
A2: For Medicare, individuals can apply through the Social Security Administration. For Medicaid, applications must be submitted to the state Medicaid agency.
Q3: What are the income limits for Medicaid if I live in a state that has expanded its program under the ACA?
A3: In states that have expanded Medicaid, you are eligible if your income is below 138% of the Federal Poverty Line. This percentage translates to an annual income of approximately $18,754 for an individual or $24,860 for a family of three in 2024.
Q4: If I am over the income limit for free Medicare, what options do I have?
A4: If your income exceeds the limits for subsidized Medicare Part B and Part D, you will need to pay higher premiums for these parts of Medicare. These are determined by the income reported on your tax return two years prior.
To guarantee they may obtain vital medical care without excessive financial hardship, it is imperative that all individuals, particularly those who are nearing qualifying age or have limited financial resources, have a thorough understanding of these programs.
To Know More Latest Finance News then Visit – stevedigioia.com